M.L. is a very healthy 60 year old woman who presented with an episode of gross hematuria in November 2018. A CT scan indicated a bladder tumor on the left wall. The upper urinary tract was normal. Her past medical history was entirely negative. An outpatient flexible cystoscopy identified a papillary exophytic solitary tumor on the left lateral wall of the bladder. The remainder of the bladder was normal.
She underwent a transurethral resection of the tumor (Figs. 1, 2). The pathology revealed a high grade urothelial carcinoma, which had minimal invasion into the lamina propria. Muscularis propria was present and uninvolved by the tumor. The stage was thus pT1a.
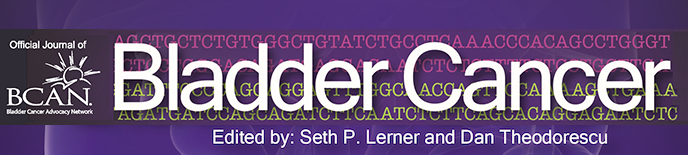
Fig. 1
Papillary tumor left wall of the bladder.
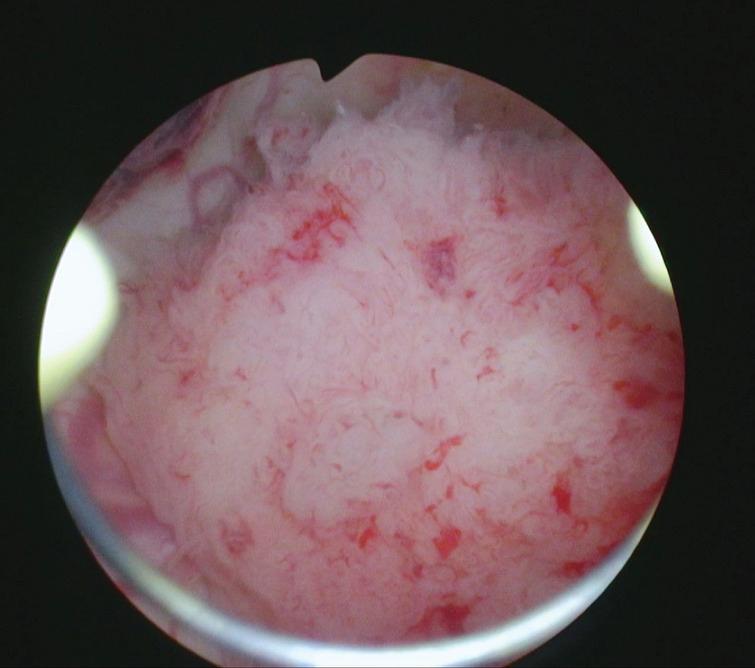
Fig. 2
Appearance of the bladder after the resection.
I considered a repeat TUR BT but after reviewing the histology with the urologic pathologist I was convinced that there was only microinvasion and a repeat resection would almost certainly find no cancer. A post TUR urine for cytology and bladder wash was negative for high grade cancer.
She received 6 weeks of BCG. This was well tolerated. A flexible cystoscopy in 1/19 identified a small cluster of abnormal urothelium in the area of the prior resection site, i.e. the left wall (Figs. 3, 4). A formal TUR of these areas was then performed (Figs. 5, 6). Most of the small “tumors” were removed with a cold cup forceps to avoid cautery artifact. The base was resected with the loop electrode. The pathology report was a nested variant of urothelial cancer with microinvasion into the lamina propria.
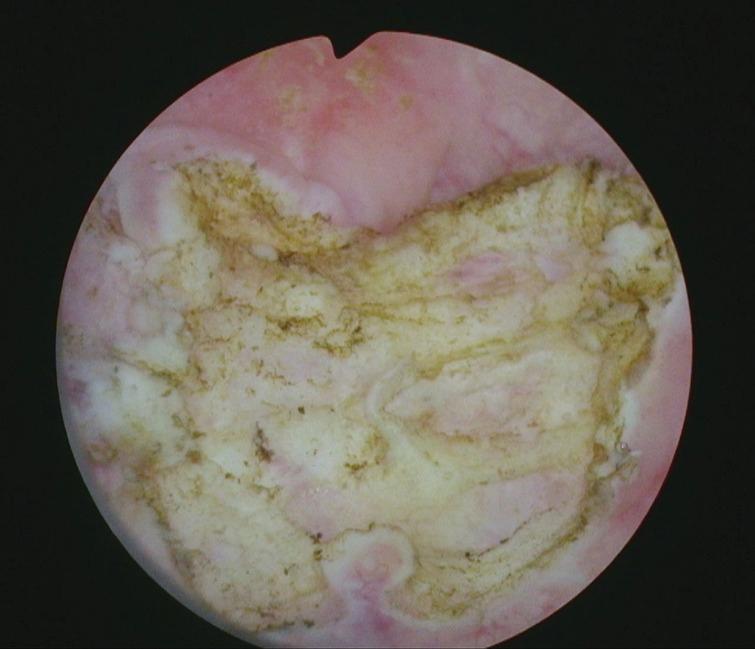
Fig. 3
Small tumor left wall seen on post BCG cystoscopy.

Fig. 4
Narrow band imaging of same area showing small tumors. They are not papillary and very small.
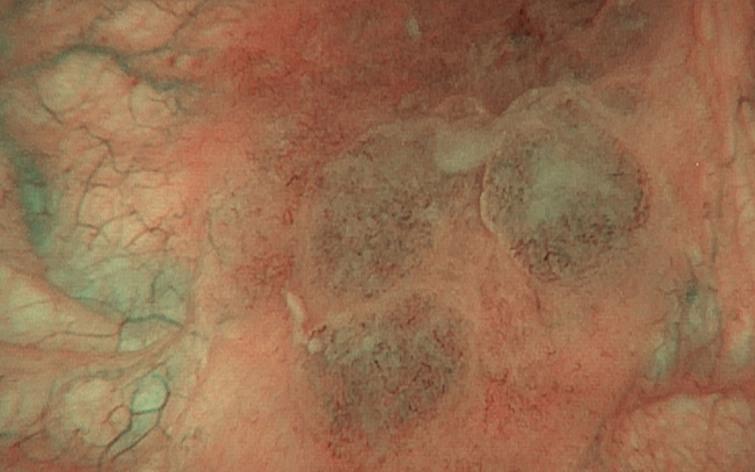
Fig. 5
Small tumors at time of resection.

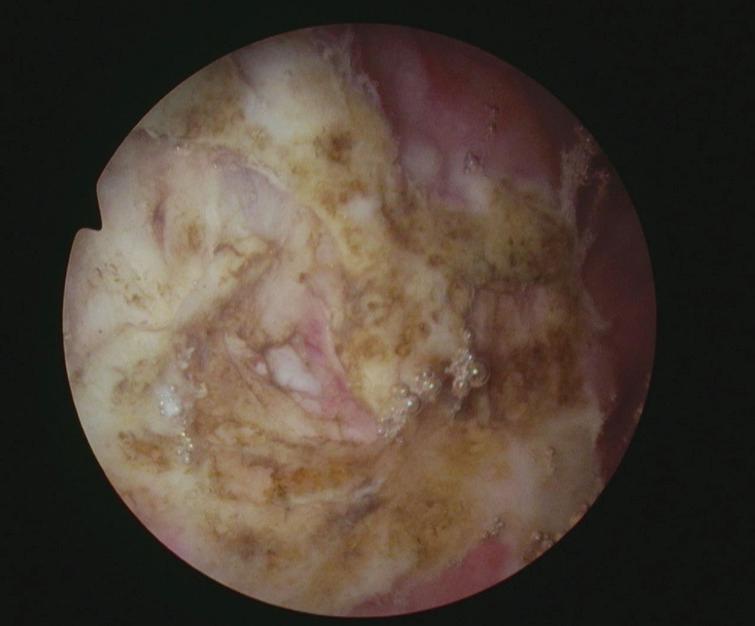
Fig. 6
Post TUR tumor bed.
This presented a difficult decision. Is the presence of a new T1 tumor despite a 6 week course of BCG sufficient to warrant a cystectomy? Is a course of intravesical chemotherapy reasonable? These were clearly very small new tumors and not a recurrence of the initial tumor. Does the variant histology, i.e. nested, dictate a different approach?
After a thorough discussion with the patient who is reluctant to proceed with removal of her bladder she has been given gemcitabine weekly for 6 weeks.
We invite our readers to review and comment on the case and management by using the online comment section below the case: https://www.bladdercancerjournal.com/challenging-cases
CONFLICTS OF INTEREST
Nothing to disclose.